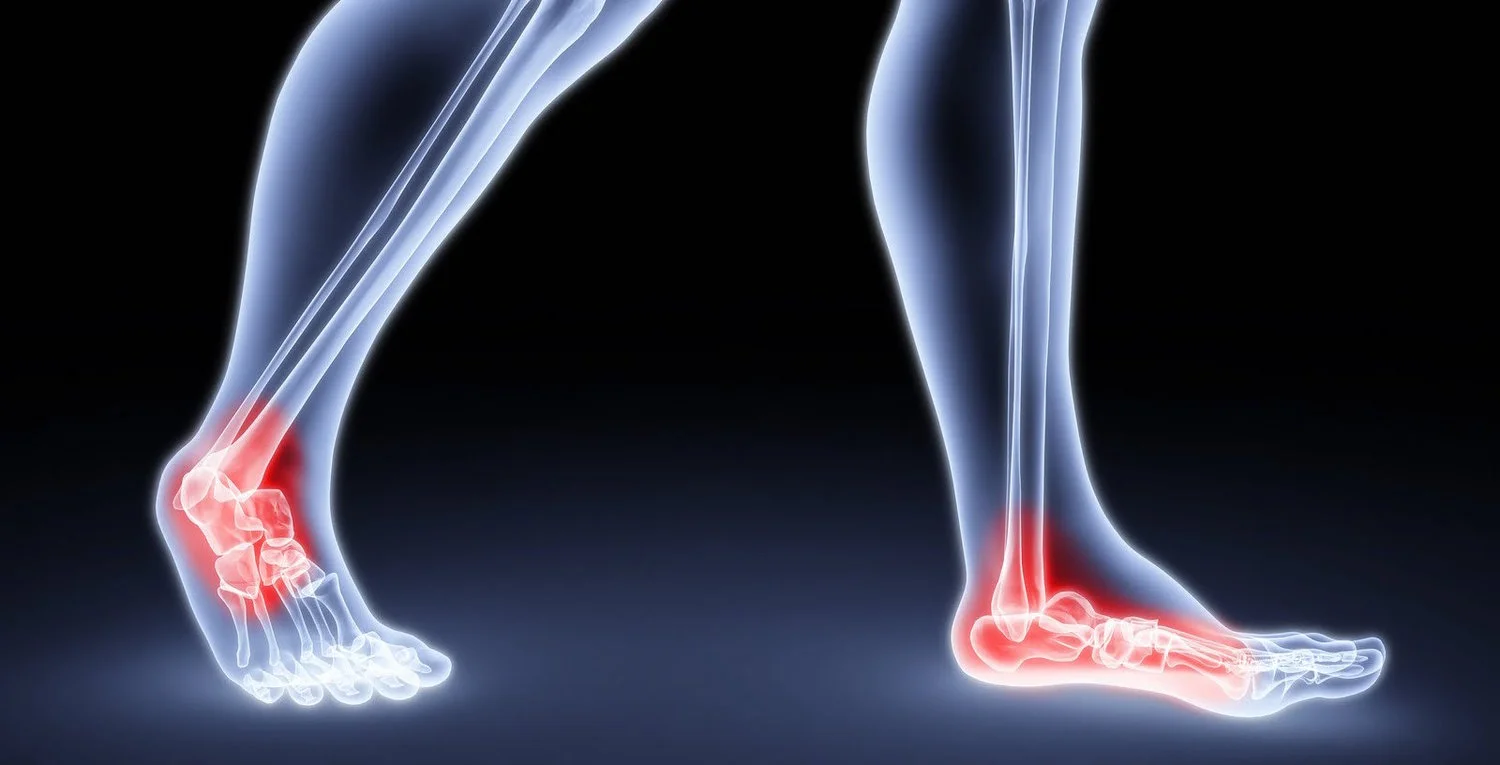
Foot and Ankle Specialists – Resources
Foot and Ankle Specialists of West Michigan created their practice to be a comprehensive foot and ankle care facility where patients can count on highly personalized care every step of the way. Below you will find articles we have published that you may find useful.